Podcast: Play in new window | Download (Duration: 33:42 — 30.9MB)
Subscribe: Apple Podcasts | RSS | More
(*Hypothetical Case)
You are an obstetrician (or anaesthetist) and you work in a peripheral hospital in a metropolitan city. You are not on call but despite this you get woken by a phone call at 2am one night. It is a junior obstetric registrar who is very keen for you to come and give them some help. They tell you the on call obstetric consultant is already busy in theatre with an urgent caesarean for fetal distress and isn’t currently available. They are on the labour ward with a women who has just had vaginal delivery of twins following a relatively long labour augmented with oxytocin. She now has an atonic uterus and despite oxytocin / ergometrine has bled about 2 litres – she has just reminded everyone that she is a jehovah’s witness and reiterates that she will not accept blood under any circumstances. Unfortunately she never had any formal antenatal discussion about blood products – this is the first time she has mentioned it! The registrar sounds very scared and they want your advice about what to do next!
What are you going to advise over the phone?
What should have been done differently in the antenatal period?
Join Graeme and I in this podcast.
Thanks to Graeme for again being a good sport and agreeing to join in this podcast to make it more of a conversation and easier to listen to! He had to ad-lib, completely off the cuff, without any warning (I literally grabbed him in the corridor).
– Tune in to find out where Wangkatjungka community is and why it is relevant to this topic!
The Most Important Points to Consider:
ANTENATAL
- Optimise the haemoglobin and iron stores before delivery
- Discuss and document what the patient will and won’t accept – make sure you understand
- Decide on the best place for delivery – consider availability of theatre and resources to manage haemorrhage (cell salvage, surgical expertise, radiology etc)
INTRAPARTUM
- stop any bleeding AS SOON AS POSSIBLE
- oxytocics – get control of tone rapidly
- Tranexamic acid – consider prophylactically or as soon as any bleeding occurs.
- theatre access immediately
- senior / experienced staff early
- hysterectomy early (not late).
- Manual aortic occlusion.
- Cell salvage – this can include vaginal bleeding and blood with amniotic fluid
POSTPARTUM
What is they have significant anaemia?
- ICU/HDU
- give oxygen
- give haematinics (iv iron / EPO) to rapidly replace the lost Hb
- minimise any further blood loss – including iatrogenic blood tests!
- paralysis & ventilation – usually needed around Hb 30-40g/L
- hyperbaric O2 – case series and reports of successful use
- polymerised Hb – can be accessed for compassionate use but manufactured in the US
USEFUL RESOURCES
- Best Reference on this topic:
- Kidson-Gerber, G., Kerridge, I., Farmer, S., Stewart, C. L., Savoia, H. and Challis, D. (2016), Caring for pregnant women for whom transfusion is not an option. A national review to assist in patient care. Aust N Z J Obstet Gynaecol, 56: 127–136. doi:10.1111/ajo.12420
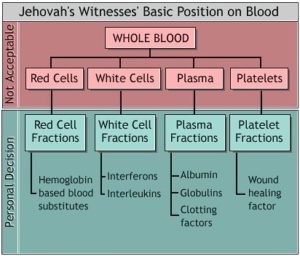
- For a good explanation and diagram explaining the Jehovah’s witnesses’ basic position on blood and blood products :
http://ajwrb.org/watchtower-approved-blood-transfusions
Tranexamic Acid
- Tranexamic acid for prophylaxis in Caesarean
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5228660/
- Tranexamic Acid for PPH
Hyperbaric Oxygen to treat severe anaemia in a JW after abruption:
https://www.ncbi.nlm.nih.gov/pubmed/23380087
Case report of use of hemopure for postpartum anaemia
https://www.tandfonline.com/doi/pdf/10.1080/22201173.2009.10872581
Case report of the use of hemopure in severely anaemic JW trauma patient in Melbourne
Vaginal Cell Salvage
Cell salvage for postpartum haemorrhage during vaginal delivery: a case series
http://www.bloodtransfusion.it/articolosing.aspx?id=000944
Is Cell salvaged vaginal blood suitable for reinfusion?
https://www.ncbi.nlm.nih.gov/pubmed/25659518
What would you do if you had one of these cases (Apart from call in sick!)Want to test the neurons more?
- 1 -A woman who has had 2 previous caesareans and who is refusing all blood products on religious grounds is booked for caesarean at your hospital. She presents at 32 weeks gestation after a 100ml antepartum haemorrhage. An ultrasound shows evidence of an anterior major placenta praevia overlying her previous caesarean scar and sinister signs indicating probable placenta percreta. Her Hb is 95 and ferritin 9.
- 2 – A woman with severe pre-eclampsia and HELLP syndrome is sent to your hospital at 32 weeks gestation. She refuses all blood products on religious grounds. She has platelets of only 20, a Hb 103, and at this stage a normal INR, APTT and fibrinogen of 2.8 . The obstetric team want to do a caesarean as they don’t think the baby will tolerate labour.
- 3 – You are in a small district hospital in Africa with limited resources and no transfusion facilities. A woman is brought in on the back of ute following delivery of twins in her village at home. She is very pale has an atonic uterus and is bleeding.
- 4 – A 65yr old woman is diagnosed with probable advanced ovarian cancer and the surgical team would like to perform a midline laparotomy and debulking. She is a Jehovah’s witness and will not accept any blood products but will accept cell salvage (what about using this in the presence of cancer?) She has a Hb 109 but to make matters difficult she has recently been started on dabigatran for a pulmonary embolus – and is also on aspirin & clopidogrel after she had a TIA 3 years ago…..